
Non-Traditional Pain Management
This document is for informational and educational purposes only and is not a substitute for medical advice, diagnosis, or treatment provided by a qualified health care provider. All information contained in this document is protected by copyright and remains the property of ProCare HospiceCare. All rights reserved.
Pain is a common and debilitating symptom experienced in our hospice and palliative care patients.

There are three distinct types of pain, including:
- Nociceptive: Localized, consistent pain; tissue damage/ inflammation
- Neuropathic: Caused by nerve damage; follows nerve pathways; described as episodic numbness, tingling, burning or stabbing pain
- Nociplastic: Centralized and widespread pain syndrome; chronic overlapping type pain conditions (ie fibromyalgia)
Nociplastic pain is a more recently utilized term. The International Association for the Study of Pain (IASP) officially adopted the term in 2018 as a “third mechanistic descriptor” of chronic pain to “more fully characterize the known pathophysiological mechanisms of pain.”
There are several reasons why clinicians and patients or their family members steer toward the non-traditional/alternative medicine route vs. the standard of care for pain management (medications including opioids, NSAIDs or acetaminophen). These reasons include adverse reactions (drowsiness is typically number one, followed by constipation and nausea), safety concerns (fall risk), the fear factor (morphine in particular), lack of efficacy (despite escalating doses), abuse/misuse, and overall patient preference.
There are several therapy types available for non-traditional pain management:
Medication Therapies
If the patient/family is hesitant to try opioids or increase the dose of their current opioid regimen, potential adjuvant medications for neuropathic pain include gabapentin and antidepressants such as amitriptyline, nortriptyline, venlafaxine or pregabalin (Lyrica®). These medications are effective for nerve pain; however, they carry the risk for adverse effects such as drowsiness.
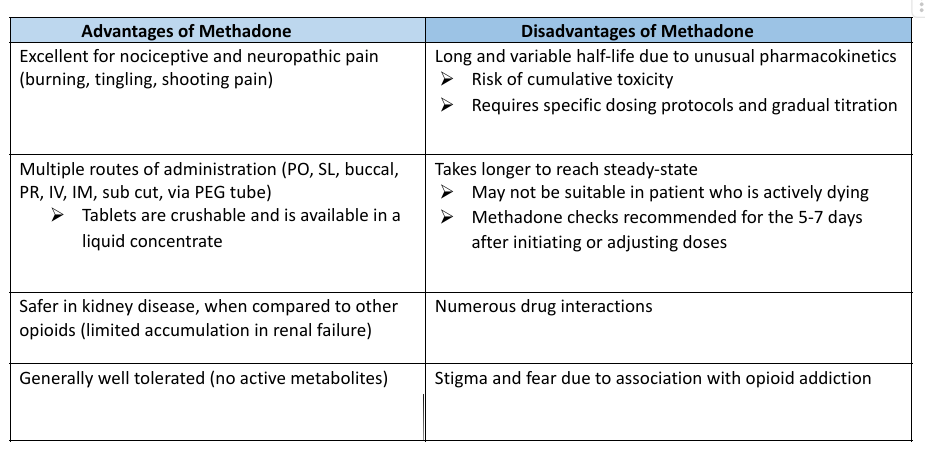
Methadone is an alternative opioid that is long acting and may help with both nociceptive and neuropathic pain due to its distinctive mu opioid agonist activity. Methadone is a synthetic opioid that is in the phenyl-heptylamine class of opioids (separate from morphine), which makes it safe to use with morphine allergies and tolerated better than traditional opioids.
Natural Therapies
Cannabis
Medical Marijuana and Cannabis have a rich and controversial history. The endocannabinoid system within the body regulates the synaptic neurotransmission and is comprised of two cannabinoid receptors, CB1 (brain and CNS) and CB2 (peripheral organs/immune system). CBI receptors have a similar neurochemical and pharmacological characteristics to opioid receptors and cannabis’ analgesic effects may be mediated at the spinal cord. It has been proven effective in refractory neuropathic pain and pain associated with Multiple Sclerosis and various cancers. In studies, cannabis is significantly better than placebo, but comparable to codeine. The greatest benefits may be seen in neuropathic pain and as an adjunct to other long-acting pain regimens. Cannabis products are available in a variety of products and routes of administration, inhalation and oral routes are the most commonly used.
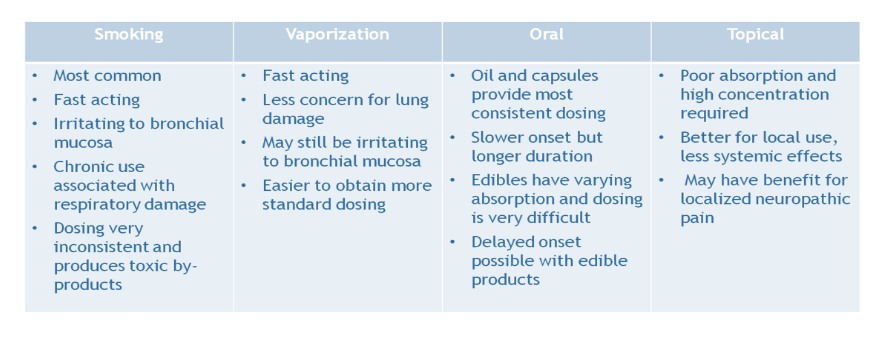
There are several notable adverse effects of cannabis use including, but not limited to: euphoria, sedation, psychosis, memory loss, hallucinations, appetite changes (could be a positive), sleep disturbances and dry mouth. Even though cannabis has become more popular in the last few years, it is still a Schedule I controlled substance (CI) federally. Due to this CI status, it cannot be prescribed legally by a physician and is subject to state-specific regulations at this time. To view your state-specific cannabis laws, visit the National Conference of State Legislature (NCSL) website at https://www.ncsl.org/health/state-medical-cannabis-laws. Keeping your state-specific laws in mind, it is best as a hospice clinician to document that your patient intends to use cannabis and provide them with evidenced-based resources to encourage safe use.
Aromatherapy
- Essential oils are FDA classified as “cosmetics”
- Knowledge is key to proper use for patient, family, and nurse
- Safety concerns: toxicity (oral or inhaled), chemical burns, flammability
- Potential benefits for hospice/palliative care
- Pain Management
- Nausea/Vomiting
- Anxiety/Stress
- Insomnia
Integrative Therapies
- Meditation
- Most studied technique = Mindfulness-based stress reduction (MBSR)
- Generally safe with no reported adverse effects
- Mental activity can influence physiologic function
- Not specifically helpful for pain, but showed promise for emotional wellbeing, anxiety, depression, and stress
- Massage Therapy
- Swedish massage using specific strokes used most often in cancer patients
- Also reflexology, deep tissue massage, shiatsu
- Studies show modest improvement in pain scores
- Safety concerns (use a trained massage therapist): Avoid pressure around tumor or bone metastases sites; implanted pumps, areas of wound or skin breakdown, sensitive skin after radiation
- Acupuncture
- Founded from Traditional Chinese Medicine practices
- Method: Use of filiform needles inserted on body in specific areas and stimulated with manual manipulation (twist, pull, or push), heat or electrical pulses
- Systematic reviews show a significant reduction in pain intensity of acute/chronic low back pain vs. placebo
- Cancer pain: equivalent or superior to oral pain medications
- Safety concerns: Pain/bleeding during needling
Based on the best available evidence, refractory pain is best managed with a combination of pharmacological and non-pharmacological type therapies. Adverse reactions and side effects can limit use of opioid or adjuvants for pain management. It is important to respect individual patient values and find that delicate balance between traditional medicine and complementary methods to achieve patient-centered care at end of life.
References
Zeng YS, Wang C, Ward KE, Hume AL. Complementary and Alternative Medicine in Hospice and Palliative Care: A Systematic Review. J
Pain Symptom Manage. 2018 Nov;56(5):781-794.e4. doi: 10.1016/j.jpainsymman.2018.07.016. Epub 2018 Aug 2. PMID: 30076965.
Moaleji, N. and Pangarkar, S. (2016, April). Oral Methadone Dosing Recommendations for the Treatment of Chronic Pain. Retrieved
from:
https://www.pbm.va.gov/PBM/clinicalguidance/clinicalrecommendations/Methadone_Dosing_Recommendations_for_the_Treatment_o
f_Chronic_Pain_July_2016.pdf
Habershaw, A. (2012, May). Methadone and QTc Prolongation. Retrieved from
https://www.urmc.rochester.edu/medialibraries/urmcmedia/medicine/palliativecare/patientcare/documents/methadoneandqtcprolong
ation.pdf
Reddy S, Hui D, El Osta B, et al. The Effect of Oral Methadone on the QTc Interval in Advanced Cancer Patients: A Prospective Pilot Study.
J Palliative Med. 2010;13:33-38.
Krantz MJ, Martin J, Stimmel B, et al. QTc Interval Screening in Methadone Treatment. Ann Intern Med. 2009;150:387-395.
Wong, E. (2013, January). A review of common methods to convert morphine to methadone. Retrieved from
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3715153/
Osvaldo, Jose. (2015, March). Revisiting methadone: pharmacokinetics, pharmacodynamics and clinical indications. Retrieved from
http://www.scielo.br/scielo.php?script=sci_arttext&pid=S1806-00132015000100060
Gagnon B, Almahrezi A, Schreier G. Methadone in the treatment of neuropathic pain. Pain Res Manag. 2003;8:149-154.

READY TO START A CONVERSATION?
Request a Live Demo and Find Out How Your Organization can be ‘Powered by ProCare Rx’
All Rights Reserved | Burgess Information Systems







