Treatment of Insomnia at End of Life
This document is for informational and educational purposes only and is not a substitute for medical advice, diagnosis, or treatment provided by a qualified health care provider. All information contained in this document is protected by copyright and remains the property of ProCare HospiceCare. All rights reserved.
Treatment of Insomnia at End of Life
Insomnia is defined as issues falling asleep or staying asleep, frequent nighttime awakenings with trouble returning to sleep despite best efforts for proper sleep environment, and adequate opportunity to sleep. It has detrimental effects on mood, normal daytime functioning, and alertness. Types of insomnia are based on symptom duration and include episodic (symptoms for at least one month but less than 3 months), recurrent (two or more episodes in a year), and persistent (lasting more than 3 months).
Causes of insomnia include the following:
- Lifestyle: Shift work, “night owl” personality, frequent napping, weeknight/weekend/routines
- ‘Activating’ Medications: Antidepressants, diuretics, nebulizers/theophylline, decongestants, corticosteroids, anticonvulsants, thyroid supplements
- Comorbid Conditions: Anxiety, uncontrolled pain, infections, GERD, breathing issues, restless legs syndrome (RLS)
- Environmental: Noise levels, partner snoring, recent move/travel
The insomnia cycle can be an endless loop if a timely intervention does not occur. The stress of clock watching, tossing/turning in bed, hitting the snooze button, and taking lengthy naps during the day can lead to the same trouble sleeping the next night. A differential diagnosis is often necessary to determine and treat the cause of sleeping issues. All of these conditions listed here and more can lead to insomnia:
- Narcolepsy: Excessive daytime sleepiness with sudden muscle weakness
- Sleep apnea: Brief periods where breathing stops and starts that result in sleep interruption and daytime drowsiness; must wear appliances to help correct breathing
- RLS: Painful sensations in lower legs that are relieved by movement and can make it hard to fall asleep/relax
- Substance Abuse: Opioids and alcohol can greatly affect sleep
- Depression: Ruminating thoughts/anxiety
Insomnia Treatment Strategies
Insomnia treatment requires a multifaceted approach and can include lifestyle modifications, cognitive behavioral therapy, and/or medications (over-the-counter (OTC) or prescription).
Lifestyle Modifications can be made to adjust poor habits, sleep environment, and/or the patient’s nighttime routine. It’s recommended by experts to get outside in the daylight, limit alcohol and caffeine intake, avoid eating for up to 3 hours prior to sleep, and limit the bedroom to sleep only (avoid use of phones/tablets). Create an environment that is conducive to sleep by choosing a comfortable mattress, pillows/bedding, keep the room at a comfortable temperature, block out light and noise and utilize scents that are light and relaxing. It also is best to have a routine to set yourself up for a good night’s rest. Keep to a consistent sleep/wake schedule, relax for thirty minutes prior to sleep, dim the lights and, most importantly, if you are unable to sleep, get up and try again later.
Cognitive behavioral therapy (CBT) focuses on negative attitudes, dysfunctional behaviors, and beliefs that lead to insomnia. It may be more effective than medications, with less adverse effects reported. Treatments include sleep restriction, stimulus control, keeping a sleep diary, relaxation therapy, and sleep hygiene education. Barriers to use of CBT are the intensity of the therapy for a hospice/palliative care patient and insufficient providers with required expertise.
Over-the-counter (OTC) sleep aids such as diphenhydramine and doxylamine may be beneficial for the short-term treatment of insomnia, but are not recommended for longer-term use due to anti-cholinergic side effects such as confusion and urinary retention, and possible exacerbation of conditions such as benign prostatic hyperplasia (BPH), asthma, cardiovascular disease, benign prostatic hyperplasia (BPH), and glaucoma.
OTC Dietary supplements have gained popularity including Melatonin. This sleep aid helps to control/reset natural circadian sleep rhythms with a wide dosing range of 0.1 to 5 mg at bedtime. Melatonin is recommended for short-term use only and may be stopped once the patient has noticed sleep improvements (proper sleep rhythms restored).
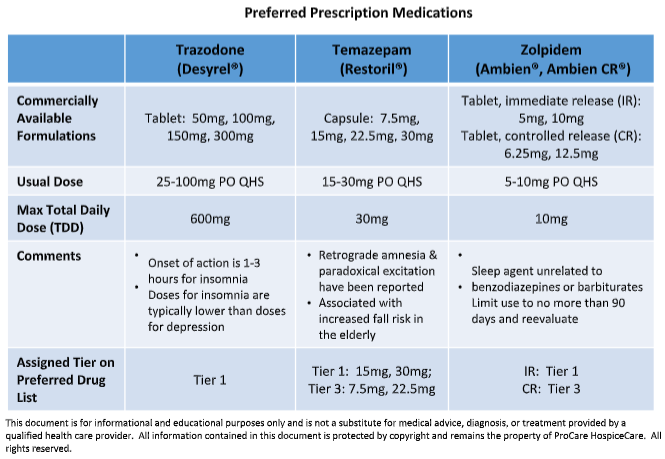
Prescription classes for insomnia include benzodiazepines (temazepam), hypnotics (zaleplon, zolpidem, eszopiclone) antidepressants (Trazodone, Mirtazapine) and newer classes such as orexin receptor antagonists (Belsomra®). Below are the preferred medications on the preferred drug list for cost and efficacy.
Insomnia can be a challenging symptom to manage at end of life amidst the other factors at play. Consider utilizing lifestyle modifications as first-line, and medications sparingly. With the understanding that medications have their limitations at end of life and as always, keep the patient and family goals of care in mind.
References
- Kasbekar R and Ambizas EM. Helping People Manage Insomnia. US Pharm. 2022;47(1):4-12.
- Davies A. Sleep problems in advanced disease. Clin Med (Lond). 2019 Jul;19(4):302-305. doi: 10.7861/clinmedicine.19-4-302. PMID: 31308108; PMCID: PMC6752246.
- Corvino M and Swanson C. Overview of Insomnia Pharmacotherapy. CorConsult Rx Podcast. [Online] Available by subscription from: https://myportal.freece.com/course/details/9a2f8e7c-80bd-4cbe-b7d9-40d234194246/446c48da-f681-4bbf-809c-97336a96ec23/2c5041db-ab50-4f56-91d7-a53957727690.
- Okun,M.L., Kravitz,H.M., Sowers,M.F., Moul,D.E., Buysse,D.J., & Hall,M. (2009). Psychometric evaluation of the Insomnia Symptom Questionnaire: A self-report measure to identify chronic insomnia. Journal of Clinical Sleep Medicine, 5(1), 41-51. [Online] Available from: https://sleep.pitt.edu//wp-content/uploads/Study_Instruments_Measures/ISQ-article.pdf.
- Wilhelm M. Sleep and Stress: Pharmacist Insights on Non-Prescription Treatment Options. PowerPak. [Online] Available from: https://www.powerpak.com/course/content/122306.
- LexiComp. Wolters Kluwer Health, Inc. Riverwoods, IL. Accessed December 2023.
- Hospice Medication Utilization Guidelines. ProCare Hospice Care. Insomnia. Available Online with registration from: https://phc.procarerx.com/docs/hugs/Section%20Three%20Symptom%20Management%20Algorithms.pdf.