October 21, 2022
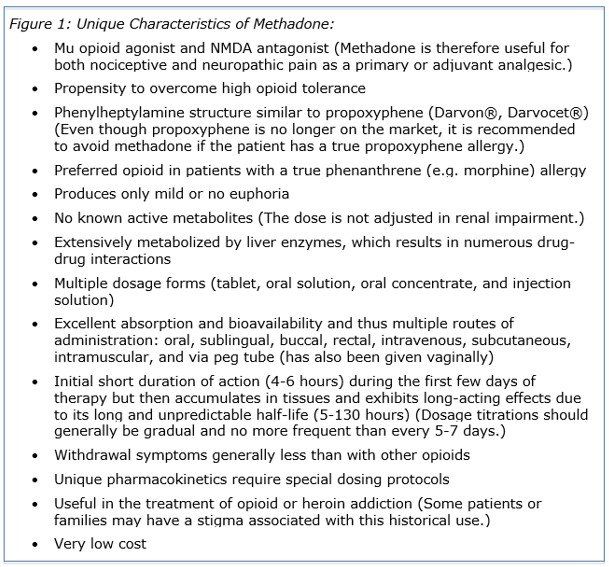
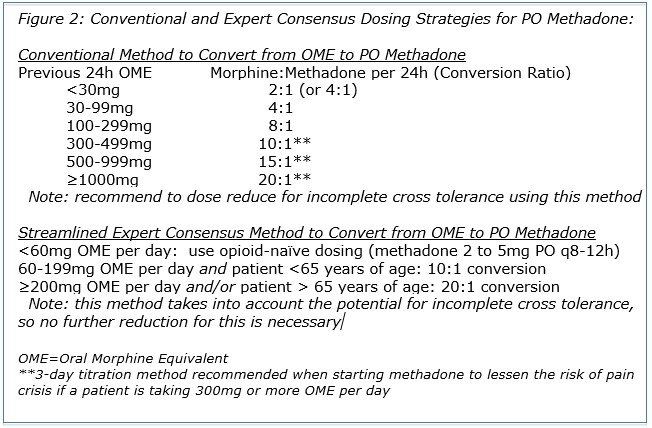
Renal impairment is relatively common in both the elderly and hospice patients, and it can affect the way medications act in the body in several ways. Most commonly, it results in decreased clearance of renally-excreted medications, leading to accumulation of the drug and/or its metabolites and subsequent adverse or toxic effects. The absorption of oral medications may be reduced in patients with renal impairment due to increased gastric pH and gut wall edema. Uremia caused by renal impairment can increase sensitivity to medications that act on the central nervous system (CNS), as well as increase the risk of hyperkalemia due to potassium-sparing drugs. In addition, uremia can enhance the potential for NSAID-induced edema or GI bleeding. Renal impairment can also lead to edema or ascites, cachexia, dehydration, decreased albumin levels and binding capacity, and decreased tissue binding, all of which can impact the effects of medications. To compensate for these renal impairment-induced changes in drug disposition, the typical actions taken regarding medication administration are to decrease the dose, increase the dosing interval, or a combination of the two. The action that would be recommended depends on the drug and its specific characteristics. There are many medications that require dose adjustment in renal impairment, but here we’ll be discussing just those that are most often seen in hospice. The goal is to make you aware of these common medications (and categories) that often need dose adjustment so they trigger a mental alert for possible follow-up if they are ordered for your patients with decreased renal function. Opioids: Many opioids can accumulate in renal impairment as the parent drug and/or metabolites. Tramadol has a maximum daily dose in all patients, but in patients with a creatinine clearance (CrCL) less than 30 mL/minute, this maximum dose is reduced to 200 mg per day and the dosing interval should be extended to every 12 hours. Morphine renal dose reductions start with a CrCL less than 60 mL/minute, with possible extension of the dosing interval at this point as well. It is typically recommended to start considering alternatives to morphine in patients with a CrCL less than 30 mL/minute, and to avoid it altogether in patients with a CrCL less than 15 mL/minute. At end of life, the benefits of morphine can sometimes outweigh the risks. Because the presentation of renal accumulation-based adverse effects may be delayed, morphine can be used even in severe renal impairment or renal failure when the prognosis is hours to days, or in dialysis patients when death is imminent. Typically, oxycodone and hydromorphone are considered preferred alternatives to morphine in patients with significant renal impairment, although they both have metabolites that can accumulate in renal failure. As a result, the dose of oxycodone should be reduced and the dosing interval increased in patients with a CrCL less than 60 mL/minute, and oxycodone extended-release products should usually be avoided in patients with a CrCL less than 30 mL/minute. Hydromorphone dose reduction is also recommended when CrCL is less than 60 mL/minute; further dose reduction and extension of the dosing interval is recommended for hydromorphone when CrCL is less than 30 mL/minute. Although hydrocodone and its active metabolites may accumulate in renal impairment, there are no dose reductions for hydrocodone/acetaminophen according to the manufacturer’s labeling. Hydrocodone extended-release products (Hysingla ER®, Zohydro ER®) are rarely used in hospice, but dose reductions are recommended in patients with moderate to severe renal impairment. Methadone and fentanyl patch are considered among the safest opioids in renal impairment because they do not have active metabolites. However, renal impairment can still alter how fentanyl moves in the body, so dose reduction is recommended in patients with a CrCL of 50 mL/minute or less. For methadone, dose reduction is not recommended until very severe renal impairment (CrCL less than 10 mL/minute). No dose reductions are recommended for buprenorphine at any degree of renal impairment, and it is generally considered safe in this population. NSAIDs: Examples of NSAIDs that are commonly used in hospice include ibuprofen (Advil®, Motrin®), naproxen (Aleve®), and meloxicam (Mobic®), and as mentioned previously, there are some concerns regarding the use of NSAIDs in renal impairment. According to the Kidney Disease: Improving Global Outcomes (KDIGO) 2012 Clinical Practice Guideline, prolonged therapy with NSAIDs is not recommended if GFR is less than 60 mL/minute/1.73m² , and NSAIDs should typically be avoided in patients with a GFR less than 30 mL/minute/1.73m². As a general rule, NSAIDs should be used at the lowest effective dose for the shortest time possible in patients with renal impairment. In addition, NSAIDs should be avoided in patients with a high risk for developing acute kidney injury (e.g. volume depleted, elderly, and/or taking other nephrotoxic medications), and should be discontinued if acute kidney injury occurs during use. Antimicrobials: Many antimicrobials require dose reduction and/or extension of the dosing interval in renal impairment. Specific dosing recommendations depend on the antimicrobial in question and the type of infection being treated. When used for multiple doses, the dose of the antifungal fluconazole (Diflucan®) should be reduced in patients with a CrCL of 50 mL/minute or less. Examples of antibiotics commonly used in hospice that need dose adjustment include: sulfamethoxazole/trimethoprim (Bactrim®); fluoroquinolone antibiotics, including ciprofloxacin (Cipro®) and levofloxacin (Levaquin®); certain penicillin antibiotics, such as amoxicillin and amoxicillin/clavulanate (Augmentin®); and some cephalosporins, including cephalexin (Keflex®) and cefdinir (Omnicef®). Nitrofurantoin (Macrobid®, Macrodantin®) also has significant concerns in renal impairment. According to the manufacturer’s prescribing information, it is contraindicated in anuria, oliguria, or significant renal impairment (defined as a CrCL less than 60 mL/minute or clinically significant elevated serum creatinine). However, limited data suggest it is safe and effective for short-term use in patients with a CrCL of 30 to 60 mL/minute, although there appears to be an increased risk of pulmonary adverse events when eGFR is less than 50 mL/minute. In any case, nitrofurantoin should be avoided altogether in patients with a CrCL less than 30 mL/minute, due to the risk of pulmonary toxicity, hepatotoxicity, and peripheral neuropathy. Renal impairment can affect drug disposition in several ways, often increasing the risk of adverse and toxic effects. Whenever you have a patient with renal impairment, evaluate whether they are taking medications that may be cause for concern and require dose adjustment, and remember that hospice clinicians, pharmacists, and drug information resources can help by providing specific renal dosing recommendations. By Joelle K. Potts RPh, PharmD, BCGP REFERENCES: Aging and Kidney Disease. National Kidney Foundation. Available at: https://www.kidney.org/news/monthly/wkd_aging [accessed 8/8/2022] Aronoff GR, Bennett WM, Berns JS, Brier ME, Kasbekar N, Mueller BA, et al. Drug Prescribing in Renal Failure: Dosing Guidelines for Adults and Children. 5th American College of Physicians, Philadelphia, PA; 2007. Renal Impairment. Chapter in: Palliative Care Formulary, 7th Edition (PCF7). Wilcock A, Howard P, Charlesworth S, Eds. Pharmaceutical Press, London, UK. Chapter 17, added April 2017; 715-35. Drug monographs. Lexcomp Online, Lexi-Drugs Online. Waltham, MA: UpToDate, Inc. https://online.lexi.com. O’Connor NR, Corcoran AM. End-stage renal disease: symptom management and advance care planning. Am Fam Physician. 2012; 85(7): 705-10. Kidney Disease: Improving Global Outcomes (KDIGO). KDIGO 2012 clinical practice guideline for the evaluation and management of chronic kidney disease. Kidney International Supplements. Jan 2013; 3(1). Available at: www.kidney-international.org Macrobid® Prescribing Information. Proctor and Gamble Pharmaceuticals, Inc. Cincinnati, OH. Revised Jan 2009. Available at: https://www.accessdata.fda.gov/drugsatfda_docs/label/2009/020064s019lbl.pdf [accessed 6/13/2022] Macrodantin® Prescribing Information. Almatica Pharma Inc. Pine Brook, NJ. Revised Mar 2013. Available at: https://www.accessdata.fda.gov/drugsatfda_docs/label/2013/016620s072lbl.pdf [accessed 6/13/2022] 2019 American Geriatrics Society Beers Criteria® Update Expert Panel. American Geriatrics Society 2019 updated Beers Criteria® for potentially inappropriate medication use in older adults. JAGS. 2019; 00: 1-21